
Professional illustration about Health
What Is Dental Inclusion
Dental inclusion is all about making sure every person, regardless of their background or identity, feels welcomed, respected, and empowered within the world of dentistry. In 2026, the conversation around Oral Health has shifted beyond just clinical care—it now heavily focuses on fostering belonging and eradicating health disparities through intentional strategies within the dental workforce and care environments. According to ongoing initiatives by the American Dental Association and other leading organizations, dental inclusion means more than just opening doors; it requires actively cultivating diversity and cultural competence in dentistry, so patients receive equitable care and professionals feel valued for their unique contributions.
At its core, dental inclusion addresses systemic barriers in Dental Education, Dental Hygiene Programs, and Dental Career Pathways. For example, schools and training programs are prioritizing minority representation in dentistry and making admissions more accessible for underrepresented groups. This includes providing scholarships, mentorship opportunities, and culturally responsive oral health education. Dental clinics are redesigning their spaces and workflows to create inclusive dental environments, ensuring that dental assistants, dental hygienists, dentists, and other dental professionals can collaborate in team-based dental care where everyone’s perspective is valued.
In real-world practice, inclusive dental care means adapting communication styles and preventive strategies to meet the needs of diverse populations. Patient-centered communication is critical, especially for those whose first language isn’t English, or who come from communities that have historically lacked access to dental services. For instance, some dental public health initiatives now include community outreach programs in languages spoken by recent immigrants, and dental clinics are hiring staff with specialized training in dental laboratory technology and dental therapy to better address the needs of patients with disabilities or chronic conditions.
Workforce diversity is another pillar of dental inclusion. In 2026, more dental students from diverse racial, ethnic, and socioeconomic backgrounds are entering Dental Education Programs thanks to concerted recruitment efforts. This growing diversity within the dental workforce directly impacts the quality and accessibility of dental care, leading to equitable health outcomes for patients who previously faced discrimination or neglect. Inclusive hiring practices and ongoing professional development foster professional inclusion, encouraging dental professionals to share their experiences, advocate for policy changes, and pursue leadership roles in industry organizations.
Dental inclusion also influences how clinics promote preventive dental care. By designing community outreach initiatives tailored to local populations—such as mobile dental units visiting rural areas, or school-based oral health screenings—dentistry is actively working to close gaps in health care access. Culturally competent care involves recognizing and respecting traditions, dietary customs, and beliefs that impact oral health. Providers are encouraged to learn from their patients and incorporate cultural awareness into treatment planning, which not only improves health but builds trust.
Inclusive dental care isn't a one-size-fits-all solution. It’s about creating systems that are flexible, responsive, and sensitive to individual circumstances. For example, dental clinics may offer sliding-scale fees, extended hours, or telehealth appointments to ensure everyone can access the care they need. The embrace of diversity in dentistry goes beyond numbers—it’s a commitment to oral health equity and the belief that everyone deserves a healthy smile. By championing dental inclusion, the profession is taking meaningful steps towards a future where every patient and provider can thrive, regardless of background or identity.

Professional illustration about Association
Current Trends in 2026
Current trends in 2026 highlight a transformative shift in oral health, dentistry, and related fields, with diversity, inclusion, and belonging at the heart of change. Today’s dental workforce is more varied than ever, driven by innovative strategies from the American Dental Association and forward-looking dental education programs. There's a clear focus on health equity, particularly in improving access to dental care for underrepresented and historically marginalized communities. Dental clinics now prioritize inclusive dental environments, implementing patient-centered communication and team-based dental care models that reflect the diversity of their patient populations. This approach not only enhances the patient experience, but also advances equitable health outcomes across the board.
Workforce diversity is a major priority, with dental hygienists, dental assistants, and dental laboratory technology professionals benefiting from expanded career pathways and comprehensive mentorship programs. Efforts to increase minority representation in dentistry are showing tangible progress in 2026. Dental students from a range of backgrounds are supported through scholarships, targeted outreach, and culturally competent training modules. Dental hygiene programs and dental education now regularly incorporate curriculum on cultural competence in dentistry, preparing graduates to recognize and address health disparities. These programs stress the importance of understanding social determinants of health and using inclusive strategies to foster belonging among both colleagues and patients.
Dental public health initiatives are leveraging community outreach to tackle persistent gaps in oral health equity. Preventive dental care campaigns are more integrated, with partnerships spanning schools, community centers, and faith-based organizations. Dental clinics frequently deploy mobile units or pop-up services to reach underserved urban and rural populations, making equitable care more accessible than ever. Technology also plays a vital role: In 2026, tele-dentistry and AI-driven patient education tools are mainstream. These advances empower dental professionals to deliver evidence-based care and oral health education, regardless of a patient’s location or language preference.
Inclusive dental care is evolving, with dental therapy gaining wider recognition and adoption in both private and public settings. This broadens the scope of practice for dental professionals and helps close gaps in care. Team-based dental care is the norm, maximizing the expertise of dentists, dental hygienists, dental assistants, and dental therapists. The result is better coordination of care and improved outcomes for diverse populations. Dental laboratories and dental laboratory technology specialists are also embracing diversity in hiring and innovation—bringing different perspectives to material science, design, and patient customization.
Dental education programs now set benchmarks for professional inclusion. Admissions policies prioritize holistic review, valuing diverse life experiences alongside academic achievement. Dental students participate in interprofessional education, collaborating with peers in medicine, pharmacy, and public health to foster a culture of equity and shared responsibility. Faculty development focuses on inclusive teaching and mentorship, ensuring that all dental professionals are equipped to build welcoming environments.
Examples from 2026 spotlight the power of these trends: - A multi-site dental clinic in Los Angeles boasts bilingual dental teams and culturally tailored care plans, reducing barriers for Spanish-speaking families. - Dental hygiene programs in Atlanta partner with historically Black colleges and universities to recruit and retain students from underrepresented backgrounds. - Community health centers across Montana deliver preventive dental care and oral health education via tele-dentistry, reaching remote Native American populations. - Dental assistants participate in ongoing training focused on inclusive dental care and patient-centered communication, improving satisfaction and trust among patients.
Practical suggestions for dental professionals and organizations embracing these trends include: - Regularly assess clinic culture and policies to ensure they align with the principles of belonging, diversity, and inclusion. - Invest in ongoing professional development centered on cultural competence and health disparities. - Enhance dental education by embedding oral health equity and inclusive care modules into curricula. - Foster team-based dental care by encouraging collaboration and cross-training among all dental workforce members. - Use technology to streamline access to information, preventive services, and treatment options for diverse and underserved groups.
In 2026, the drive toward diversity, inclusion, and health equity in dentistry is not just aspirational—it’s actionable and measurable. With these current trends, dental professionals and organizations are well-positioned to deliver equitable care that truly reflects the communities they serve.

Professional illustration about Belonging
Common Types Explained
When exploring the landscape of dental inclusion in 2026, it’s crucial to understand the common types and approaches that shape diverse and equitable oral health environments. The American Dental Association has emphasized that meaningful inclusion goes far beyond simply increasing numbers—it's about fostering a sense of belonging and creating inclusive dental environments where dental professionals, patients, and students thrive. Let’s break down the different forms of inclusion as they play out across the dental workforce, education, clinics, and patient care.
1. Professional Inclusion Across Roles
Workforce diversity is at the heart of dental inclusion. This means striving for equal representation not just among dentists, but across all dental professions: dental hygienists, dental assistants, dental therapists, and professionals engaged in dental laboratory technology. In practical terms, professional inclusion shows up in hiring practices that value candidates from varied backgrounds, mentorship programs for minority dental students, and leadership development for underrepresented groups. For example, a dental clinic might actively recruit dental hygienists from communities that have historically faced health disparities, aiming to better reflect the population they serve.
2. Educational Inclusion and Pathways
Inclusive dental education isn’t just about accepting students of diverse backgrounds; it’s about supporting them throughout their journey. Dental education programs and dental hygiene programs increasingly offer scholarships, academic support, and peer mentorship to students from minority groups. Some universities have launched community outreach initiatives that connect pre-dental students with resources in underserved neighborhoods, fostering real-world oral health education and guiding students through dental career pathways. These approaches help combat barriers to health care access and nurture future leaders in dental public health.
3. Patient-Centered and Culturally Competent Care
One of the most impactful types of inclusion happens at the point of care. Inclusive dental care focuses on equitable treatment for patients, regardless of background, disability, or socioeconomic status. Dental professionals are increasingly trained in cultural competence in dentistry, helping them understand and respect their patients’ beliefs, languages, and values. Patient-centered communication builds trust and improves outcomes, especially for groups that historically have had limited access to dental care. For example, clinics may offer bilingual services or adapt their scheduling to accommodate working families, clearly demonstrating a commitment to equitable care.
4. Institutional Inclusion in Dental Clinics
Modern dental clinics are embracing inclusive dental environments by creating policies that actively welcome both patients and professionals from underrepresented groups. This can mean implementing accessible facilities for those with disabilities, accommodating religious practices for staff and patients, or establishing zero-tolerance frameworks for discrimination. At the same time, many clinics collaborate with local health organizations to expand health care access through mobile units or preventive dental care initiatives, targeting communities most affected by oral health inequity.
5. Structural Inclusion and Policy Change
On a broader scale, dental inclusion is shaped by health equity policies and systemic frameworks. The push for minority representation in dentistry isn’t just about numbers; it’s about changing institutional culture and breaking down barriers. Efforts may include revising licensure requirements to accept international dental graduates, or working with state boards to recognize more flexible dental therapy roles, which helps increase provider availability in rural and urban underserved areas.
6. Team-Based Approaches and Collaborative Care
Team-based dental care exemplifies inclusion by ensuring every role—dentists, hygienists, assistants, and laboratory technicians—contributes to decision-making and patient outcomes. This collaborative care model elevates the voices of all dental professionals and fosters a sense of belonging, which translates to better equitable health outcomes for patients. For example, a dental team might include a social worker to address barriers to oral health equity, or organize regular workshops to build cultural competence among staff.
7. Promoting Diversity in Dentistry Through Outreach
Sustained change requires ongoing community outreach and recruitment efforts by educational institutions, clinics, and professional associations. In 2026, many dental education programs partner with local schools and non-profits to introduce young people from diverse backgrounds to the possibilities within dentistry. These efforts broaden diversity in dentistry, encourage professional inclusion, and ultimately foster a health care system that is more representative and responsive.
By embracing these various types of inclusion, dental professionals and organizations are shaping a future where oral health and dental care are genuinely accessible, equitable, and culturally responsive. Each approach strengthens the entire oral health ecosystem, making belonging and diversity the norm rather than the exception.

Professional illustration about Workforce
Causes of Dental Inclusion
Understanding the causes of dental inclusion starts with recognizing the multifaceted barriers and opportunities shaping the current landscape of oral health in the United States. The American Dental Association and other professional organizations have emphasized the need for belonging and diversity in dentistry to foster health equity and reduce health disparities among different populations, but the roots of dental inclusion dig much deeper into social, educational, and systemic factors.
One of the primary drivers is the historical lack of workforce diversity in dental professions. For decades, dentistry was predominantly represented by homogenous groups, making it difficult for minority groups and individuals from underserved backgrounds to feel welcomed or valued—either as patients or as part of the dental workforce. Minority representation in dentistry remains a key concern even in 2026, affecting everything from dental education pathways to day-to-day interactions inside dental clinics. When dental professionals share a cultural background or language with their patients, they are better equipped for patient-centered communication that improves equitable health outcomes.
The evolution of dental education programs and dental hygiene programs is another significant cause shaping dental inclusion. Institutions that prioritize inclusive dental environments recruit and support students from diverse backgrounds, not only in admissions but also through mentorship and financial aid. For example, a dental school that integrates cultural competence in dentistry throughout its curriculum prepares dental students and dental hygienists to approach clinical care with sensitivity and respect for cultural differences. These educational changes ripple outward, affecting the makeup of the dental workforce and the accessibility of preventive dental care in communities that historically faced exclusion.
Community outreach efforts further influence dental inclusion. Dental clinics, public health programs, and nonprofit organizations that proactively engage with marginalized groups help bridge the gap in health care access. For instance, mobile dental clinics visiting rural or inner-city neighborhoods improve trust and rapport with local communities, introducing patients to inclusive dental care that considers individual needs and circumstances. These initiatives often highlight the importance of team-based dental care, where dental assistants, hygienists, dentists, and dental therapists collaborate to provide comprehensive and equitable care.
The structure of dental career pathways also plays a crucial role. Some professions, such as dental laboratory technology and dental therapy, are increasingly accessible to individuals from nontraditional backgrounds due to more flexible educational requirements and alternative credentialing options. This expansion is key to professional inclusion, offering entry points into dentistry beyond the traditional dentist route. As a result, dental professionals from varied backgrounds can contribute to oral health equity, bringing new perspectives to dental public health challenges and solutions.
At the systemic level, policies and leadership within organizations like the American Dental Association are critical in shaping the causes of inclusion. By advocating for inclusive dental environments and diversity in dentistry, these organizations can push for policy changes that remove barriers to licensure, support dental education reform, and encourage ongoing professional development in cultural competence. In turn, dental professionals become better prepared to serve a diverse patient base and foster a sense of belonging for their colleagues.
Practical strategies for driving dental inclusion include:
- Implementing mentorship programs for underrepresented dental students and new professionals, encouraging retention and career development within dentistry.
- Expanding scholarships and financial aid aimed at minority and low-income applicants to dental and dental hygiene schools, making dental career pathways more attainable.
- Designing community-based clinical rotations as part of dental education, so students gain firsthand experience with underserved populations and learn to tailor care strategies.
- Investing in continuing education for practicing dentists and dental assistants focused on cultural competence, implicit bias, and patient-centered communication.
- Promoting leadership opportunities for minority professionals within dental organizations and dental clinics to influence system-wide changes.
Real-world examples can be found in clinics that redesigned their waiting areas and patient intake forms to reflect greater inclusivity and diversity, improving patient comfort and decreasing anxiety—critical factors for preventive dental care uptake. Similarly, dental hygiene programs that emphasize community outreach initiatives are building networks between students and local organizations, ultimately enlarging access to equitable care.
Ultimately, the causes of dental inclusion are complex but actionable. They stem from historical inequities, educational reform, conscious community engagement, systemic policy changes, and individual commitment to belonging and diversity. Addressing these causes with specific, measurable efforts can transform the future of dentistry, leading to truly inclusive oral health for all Americans in 2026 and beyond.
Professional illustration about Dentistry
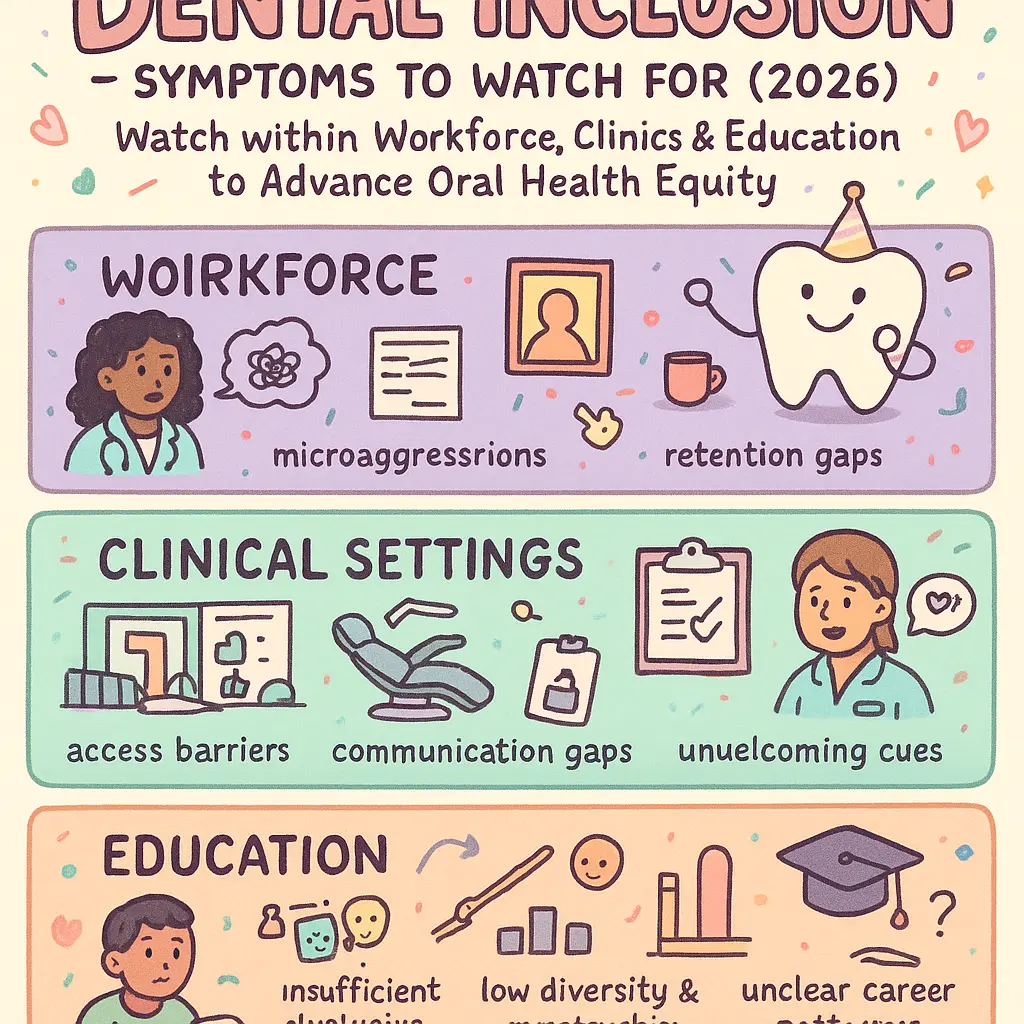
Symptoms to Watch For
When it comes to dental inclusion in 2026, paying close attention to subtle and overt symptoms to watch for within the dental workforce, clinical settings, and educational environments is crucial for fostering genuine belonging and advancing Oral Health Equity. These symptoms can manifest in various forms, ranging from patient interactions to internal team dynamics, signaling gaps in Diversity in Dentistry and areas where Health Disparities might persist. One of the most apparent signs is the underrepresentation of minorities among Dental Professionals, including Dental Hygienists, Dental Assistants, and Dentists themselves. For example, if your Dental Clinic staff lacks diversity reflective of the local community’s demographics, it may not provide equitable perspectives or culturally competent care necessary for optimal health outcomes.
On the patient side, watch for recurring patterns where certain groups consistently experience barriers to Health Care Access or voice concerns about feeling misunderstood. In today's more inclusive environment, patients may be less hesitant to express if they feel their cultural background is overlooked, or if their values are not respected during appointments. A symptom could be patients declining Preventive Dental Care, skipping appointments, or seeking care only in emergencies, which often correlates with a lack of trust or connection—an indicator that your practice may need to improve its patient-centered communication and community outreach initiatives.
Within dental education, symptoms of exclusion might show up as limited enrollment of students from diverse backgrounds in Dental Education Programs and Dental Hygiene Programs. For instance, if your admissions or recruitment materials don't actively promote diversity or your curriculum doesn’t incorporate cultural competence in dentistry, students from underrepresented groups may feel unwelcome or unsupported. The same holds true for Dental Career Pathways, where a lack of mentorship and networking opportunities can deter minority students or professionals from pursuing advanced roles in areas like Dental Laboratory Technology or Dental Therapy.
Team-based settings also merit focused attention. Symptoms to monitor here include recurring miscommunication, lack of collaborative spirit, or unequal opportunity for leadership roles among staff members of diverse backgrounds. If your staff meetings are dominated by a few voices and others routinely feel sidelined, this can be a clear marker of insufficient inclusion. Additionally, feedback mechanisms should be evaluated: Is there a system for anonymous input on inclusion? Do your Dental Public Health initiatives solicit broad participation from all team members? These questions help identify invisible barriers that may be hindering professional inclusion and equitable care.
Another practical sign involves differing health outcomes among patient groups. For example, if data reveals that oral health issues like untreated cavities or periodontal disease are disproportionately affecting specific communities served by your clinic, this may reflect underlying gaps in access to inclusive dental care. Tracking such metrics and analyzing patient feedback enables targeted improvements. The American Dental Association recommends regular audits of service delivery and patient satisfaction, ensuring that inclusive dental environments aren’t just aspirational but demonstrably effective in creating better health for all.
Proactive strategies to spot and address these symptoms include the following:
- Regular diversity audits to monitor workforce composition, leadership, and mentorship opportunities.
- Patient satisfaction surveys focusing on inclusivity and cultural sensitivity.
- Community-based listening sessions to understand unmet needs from minority populations.
- Ongoing staff training in cultural competence, anti-bias strategies, and team-based care.
- Reviewing Dental Education curriculum for representation and relevance to diverse backgrounds.
In 2026, with health equity and inclusion at the forefront of dental innovation, recognizing these symptoms isn’t just about compliance—it reflects a commitment to improving equitable health outcomes and creating a culture where every individual, from Dental Students to Dental Professionals, truly feels they belong. By staying alert to these signals and responding proactively, your dental setting can build a stronger, more inclusive foundation for advancing Oral Health and reducing Health Disparities.
Professional illustration about Diversity
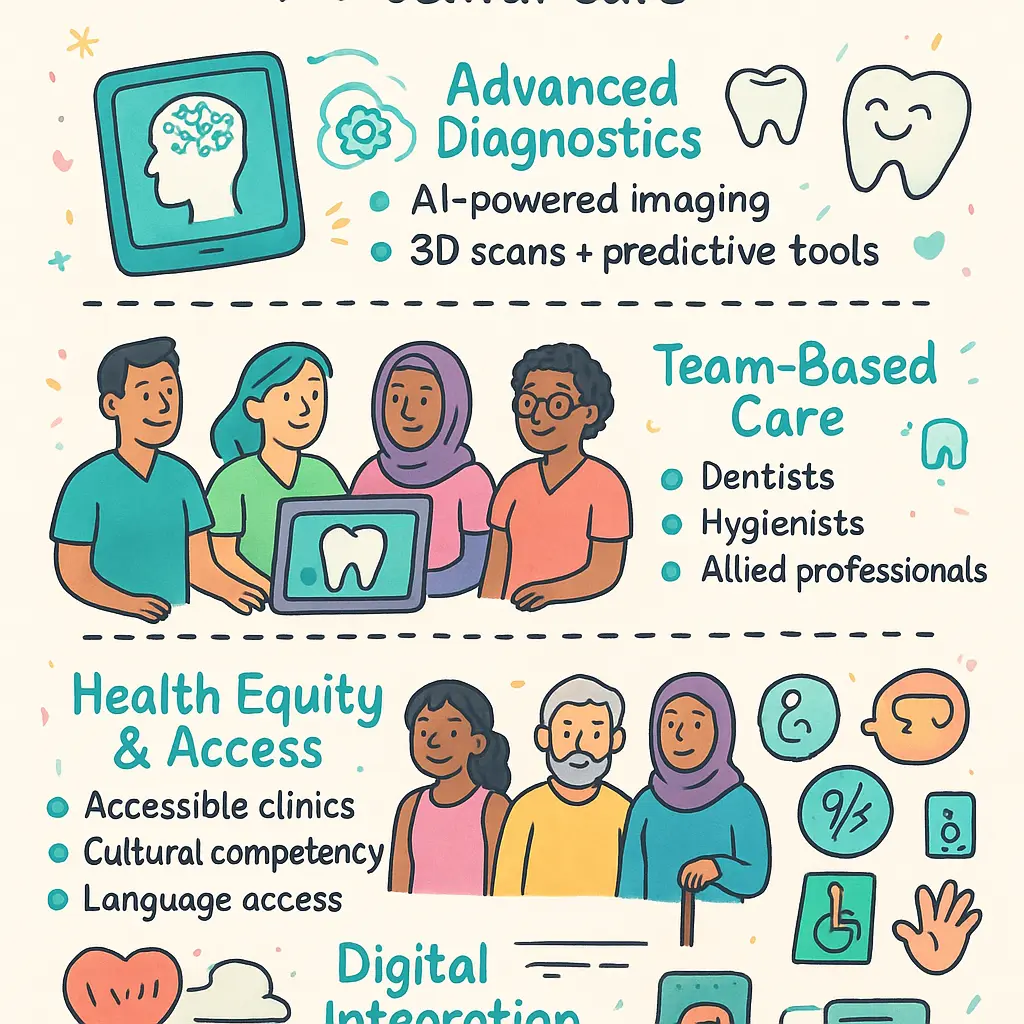
Diagnosis Methods Today
With advancements in dental technology and growing attention to health equity, diagnosis methods in 2026 go far beyond traditional chairside exams. Dentists, dental hygienists, and other dental professionals leverage integrated digital tools—think artificial intelligence-powered imaging, electronic health records, and telediagnosis—to ensure every patient, regardless of background, feels a sense of belonging and receives inclusive dental care. Today’s oral health assessment is not just about spotting cavities or gum disease—it’s about understanding the whole person, with their lived experiences and cultural context, thanks to a greater emphasis on cultural competence in dentistry.
Patient-centered communication is crucial for accurate diagnosis. Dental clinics, inspired by the American Dental Association’s latest inclusion guidelines, train staff on how to navigate language barriers and treat patients from minority communities with respect and empathy. For example, during routine exams, dental assistants and hygienists use visual aids, plain language, and interpreters when necessary, making oral health information accessible to everyone—bridging gaps created by previously overlooked health disparities. This approach reinforces the importance of diversity in dentistry and workforce diversity, catalyzing better oral health outcomes.
State-of-the-art imaging and diagnostic tools are available across many dental clinics, thanks to expanded federal and state support for health care access. These clinics employ portable X-ray devices, intraoral cameras, and even chairside 3D scanners, enabling quick, detailed images and empowering dental therapy teams to identify oral issues earlier, especially in underserved populations. Dental educators ensure dental students in dental education programs and dental hygiene programs develop expertise not only in advanced technology but also in recognizing social determinants affecting oral health—environment, nutrition, housing, and cultural beliefs all play into differential oral health equity.
Inclusive diagnostic protocols also take into account minority representation in dentistry, with teams collaborating across backgrounds to interpret findings and design personalized care plans. In community outreach settings, mobile diagnostic units and pop-up dental clinics are staffed by diverse teams—including dental assistants, hygienists, and dentists trained in trauma-informed care and screening for common diseases disproportionately affecting certain groups. This approach expands the reach of preventive dental care, catching problems early in populations previously left behind.
Another modern shift: implementing team-based dental care during diagnostic visits. Dentists now routinely consult with dental laboratory technology experts and dental public health specialists to confirm unusual findings, especially when interpreting diagnostic data from underserved and culturally diverse patient groups. This model fosters equitable care, since combined expertise minimizes missed diagnoses and supports tailored solutions—for instance, creating custom oral hygiene education programs for high-risk communities or designing special dental career pathways to bolster professional inclusion.
The diagnostic phase includes screening for systemic conditions that manifest orally, such as diabetes or heart disease, which are often more prevalent among marginalized groups. Expanded protocols, advocated by the ADA and public health experts, encourage not only dental assessment but referral to primary care, promoting truly integrated healthcare and equitable health outcomes. This larger lens enables providers to identify and address the root causes of oral health challenges, strengthening the foundation for lifelong wellness.
In 2026, the combined expertise and diversity among dental workforce members, paired with cutting-edge diagnostics and a commitment to inclusive dental environments, ensures every patient can access high-quality oral assessments. Dental professionals strive to eliminate bias and foster belonging, empowering more people to participate actively in their own care. Through ongoing innovation and education, today’s diagnosis methods set a new standard for equity and excellence in dentistry.
Professional illustration about Inclusion
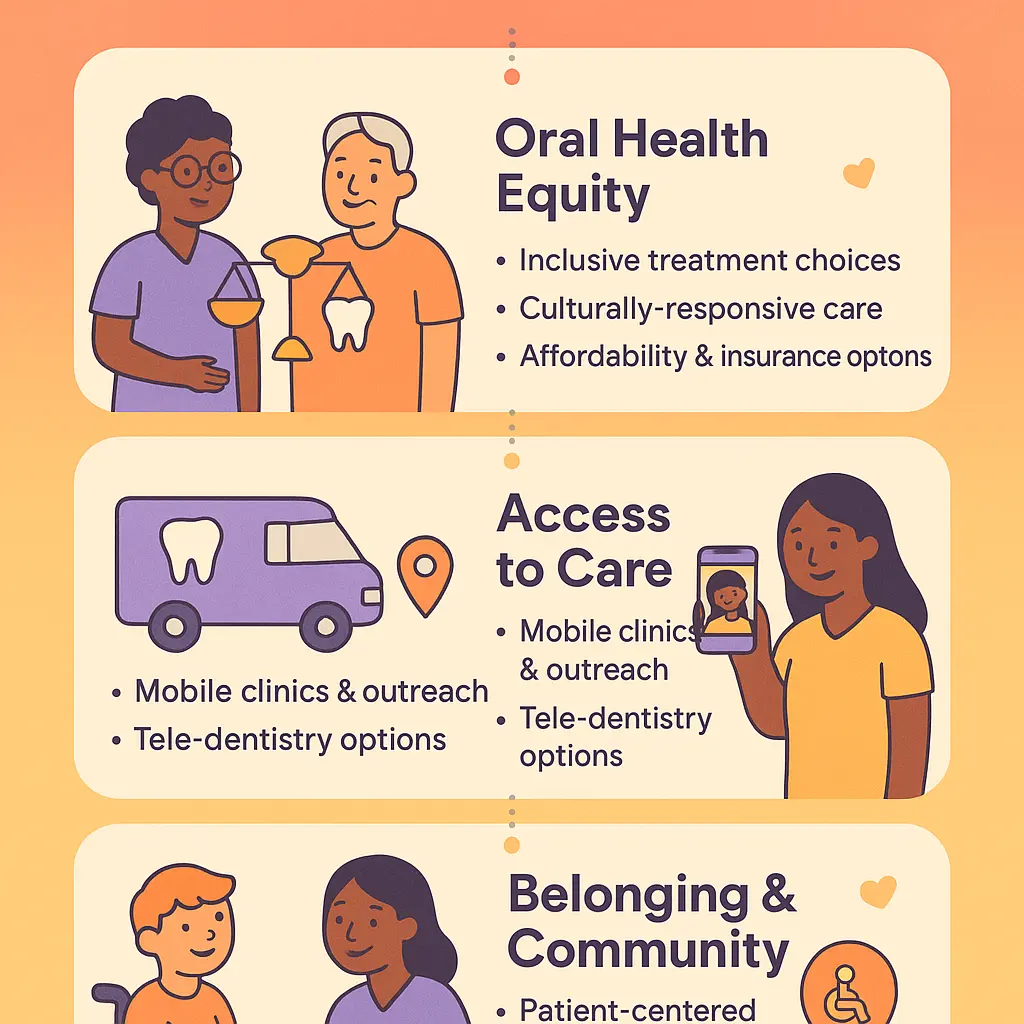
Treatment Options 2026
When it comes to Treatment Options in 2026, dentistry is making bold strides to advance Oral Health Equity, break down barriers in health care access, and reinforce a true sense of Belonging for every patient. The American Dental Association and top dental institutions now champion innovative approaches to care that blend advanced technology, workforce diversity, and elevated inclusion measures. Patients who visit modern dental clinics in 2026 experience individually tailored treatment plans that prioritize their unique needs, backgrounds, and cultural contexts—embracing true patient-centered communication and cultural competence in dentistry.
Expanding Options Through Team-Based Care
Team-based dental care is on the rise, and it's changing how treatments are delivered. Dentists, dental hygienists, dental assistants, dental therapists, and professionals trained in dental laboratory technology work hand-in-hand, each contributing their specialized expertise to improve patient outcomes. This collaborative approach means patients receive preventive dental care, restorative procedures, and community outreach all under one roof, with seamless transitions between specialists for holistic and inclusive dental care. In underserved communities, mobile dental teams extend outreach, fueled by diverse workforce representation—especially minority representation in dentistry—to bridge gaps in care access.
Cutting-Edge Technology and Equitable Care
2026 has ushered in digital dentistry innovations that directly target health disparities. Portable diagnostics, 3D printing for same-day crowns, and AI-driven risk assessments make treatments more efficient and affordable, particularly for those who previously faced barriers. Dental clinics commit to equitable care by employing these technologies in both private practices and public health settings. Through dental public health initiatives, trained providers can deliver screenings and preventive interventions in schools, senior centers, and remote communities, reducing travel and cost burdens for vulnerable individuals.
Personalized Prevention and Inclusive Environments
Preventive dentistry is being personalized like never before, with custom oral hygiene plans designed by dental professionals to fit a patient's age, ethnicity, medical conditions, and even lifestyle. The proliferation of culturally competent dental hygiene programs ensures that education, communication, and clinic settings foster inclusive dental environments, where patients feel comfortable discussing their care preferences and concerns. These environments support diverse patient populations, including immigrants, racial minorities, individuals with disabilities, and LGBTQ+ people—reflecting a commitment to equitable health outcomes and nurturing trust.
Diversity in Education and Workforce Initiatives
2026 witnessed sweeping changes in dental education and dental career pathways. New dental education programs focus not only on clinical excellence, but also on training dental students and professionals to recognize and address health disparities—including social determinants like income, language barriers, and insurance status. Scholarships, mentorships, and dedicated recruitment efforts drive diversity in dentistry, bringing in voices from all backgrounds and strengthening the profession's ability to tailor care. Dental schools now require coursework in professional inclusion, bias recognition, and community service, with students joining outreach initiatives to support marginalized populations.
Practical Strategies for Patients and Professionals
Patients seeking dental treatment in 2026 can expect choice, transparency, and advocacy throughout their care journey:
Multiple Care Settings: Treatments are available in community clinics, school-based centers, private practices, and mobile units for easy access. Transparent Payment Policies: Sliding scales, insurance support, and public health programs help break financial barriers. Patient Advocates: Dedicated staff guide minority, disabled, or non-English speaking patients through registration, insurance, and treatment discussions. Group Therapy and Interdisciplinary Support: Where appropriate, mental health services and nutritional guidance are integrated, reflecting total well-being.
Dental professionals and students are urged to pursue continuing education in cultural awareness and to actively participate in diverse teams. This not only elevates patient care, but also creates mentorship and support opportunities for next-generation caregivers.
Looking Ahead to Graduate and Advanced Training
Career advancement in dental fields is increasingly accessible. Programs in dental therapy, dental hygiene, lab technology, and public health offer flexible and inclusive admission standards, helping individuals from all backgrounds join the dental workforce. The consensus across the industry—including the American Dental Association—is that true oral health equity depends on nurturing diversity, inclusion, and belonging at every level, from training to practice to leadership. Real-world success stories are everywhere: clinics led by bilingual teams improving rural oral health, and urban outreach groups providing targeted preventive care for children of color.
In 2026, the landscape of treatment options in dentistry is more robust, diverse, and inclusive than ever before, setting a new standard for equitable and accessible oral health care nationwide. Patients and providers alike benefit from this collaborative, culturally competent, and forward-thinking approach.
Professional illustration about Dental
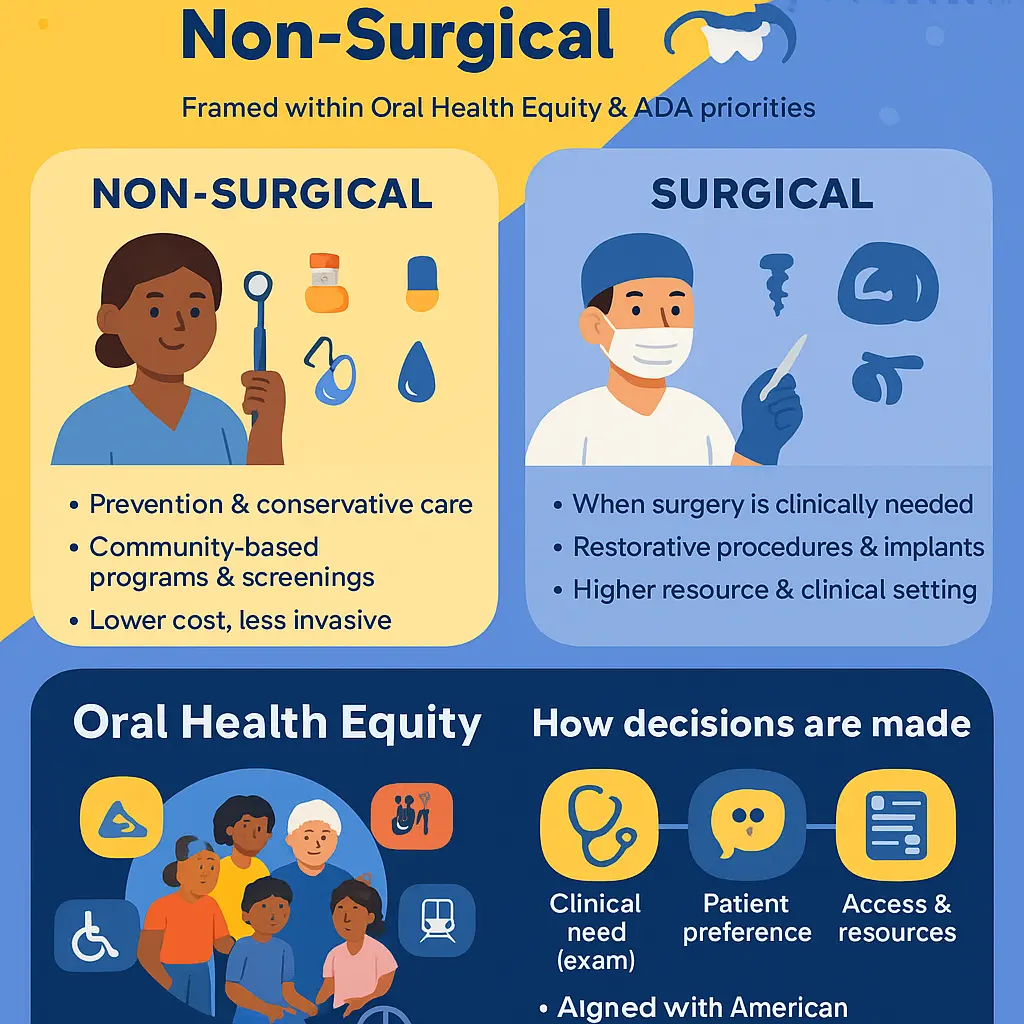
Surgical vs. Non-Surgical
When discussing surgical vs. non-surgical approaches in dentistry, it’s crucial to frame the conversation within the context of oral health equity and the current priorities established by the American Dental Association. Both treatment options serve important roles in delivering comprehensive dental care, but their application often depends on the unique needs of diverse patient populations. Non-surgical dental procedures—like preventive care, scaling and root planing, dental hygiene therapy, fluoride treatments, and sealants—are essential for promoting inclusive dental care and minimizing health disparities. These preventive and maintenance-focused treatments are most often administered by dental hygienists and dental assistants, whose expertise is developed through rigorous dental hygiene programs and supported by targeted community outreach initiatives. Particularly for marginalized or underserved groups, access to non-surgical dental care can be the foundation for belonging in the oral health system, empowering individuals to take charge of their health and participate fully in their communities.
On the flip side, surgical dental procedures—such as dental extractions, periodontal surgeries, implant placements, and oral reconstructions—represent a critical, yet resource-intensive, component of dentistry. In recent years, diversity in dentistry has become an increasingly important topic, especially concerning how different racial, ethnic, and socioeconomic groups access both surgical and non-surgical services. Equitable access to oral surgery, for example, might be influenced by a patient’s geographic location, insurance coverage, language barriers, or their ability to navigate the dental care system. This is why the integration of cultural competence in dentistry and patient-centered communication are emphasized throughout dental education programs—not only to foster greater minority representation in dentistry, but also to ensure that dental professionals understand the cultural and contextual factors that affect treatment decisions and outcomes.
From a dental workforce diversity perspective, professionals specializing in surgical fields—like oral surgeons or periodontists—often collaborate with non-surgical providers in team-based dental care environments. These collaborative models uphold the values of professional inclusion and foster a sense of belonging among dental professionals of varying backgrounds and specialties. For instance, in diverse dental clinics, a patient with advanced gum disease may receive non-surgical therapy and oral health education from a dental hygienist, followed by surgical intervention from a periodontist. By designing care workflows that connect both surgical and non-surgical specialties, dental practices actively contribute to removing access barriers and achieving greater health equity.
The distinction between surgical and non-surgical interventions also highlights disparities in health care access. In parts of the United States where dental professionals are scarce—or where dental therapy and dental laboratory technology are underrepresented—patients may forgo essential non-surgical treatments until their condition requires surgery, inadvertently perpetuating health disparities. To address these gaps, the American Dental Association has advocated for expanded roles for dental therapists and dental assistants as well as broader adoption of inclusive training within dental education. These efforts directly impact equitable care and facilitate more timely, efficient pathways for dental students and future professionals to serve a wide variety of patient needs.
Inclusive dental care models prioritize early intervention using non-surgical strategies, aiming for equitable health outcomes and the reduction of advanced treatments later. However, when surgical interventions become necessary, it’s vital to ensure that workforce diversity and integrated patient-centered care principles remain central. This includes not only delivering high-quality treatment, but also understanding and respecting each patient’s background, expectations, and lived experiences. For example, dental public health initiatives now often deploy culturally sensitive educational sessions tailored for local communities, both to prevent the need for surgery and to demystify surgical procedures when they cannot be avoided.
Ultimately, the surgical vs. non-surgical divide in dental inclusion is less about the procedures themselves and more about ensuring that every patient—regardless of their background—can access the full spectrum of modern dental services. By fostering cultural competence, nurturing diverse career pathways within dentistry, and eliminating systemic obstacles to either option, the dental profession solidifies its overarching mission: to create truly inclusive dental environments where everyone has the right and opportunity to optimal oral health.

Professional illustration about Hygienists
Pediatric Dental Inclusion
Promoting Pediatric Dental Inclusion in 2026 means prioritizing belonging and health equity for every child, regardless of their background, ability, or family income. An inclusive approach calls for collaboration across the dental workforce—dentists, dental hygienists, assistants, and educators—to actively challenge health disparities and ensure equitable care in dental clinics. To effectively address these gaps, it’s crucial that professionals use patient-centered communication and develop cultural competence in dentistry, so children from diverse communities feel confident and respected.
A practical strategy to foster inclusion starts with integrating diversity in dentistry within dental education programs. The American Dental Association strongly advocates for expanding access to education, encouraging minority representation among dental students and across dental career pathways such as dental therapy or laboratory technology. In 2026, many dental hygiene programs emphasize workforce diversity, offering mentorship and scholarships for underserved youths. By creating pathways for students from underrepresented groups, the future workforce becomes more culturally sensitive, driving professional inclusion for pediatric patient populations.
Dental public health initiatives in the United States now emphasize community outreach, connecting with families in rural or urban areas who typically face the steepest barriers to quality oral health. Mobile dental vans, bilingual care teams, and events co-organized with schools exemplify how inclusive dental care can reach young children where they live and learn. These clinics routinely adapt facilities to welcome children with disabilities, offering sensory-friendly environments, visual communication aids, and trained staff specialists, thus ensuring all children feel safe and valued.
Preventive dental care is another keystone of pediatric inclusion. Dental professionals are incorporating customized plans that respect both cultural beliefs and family realities—whether it’s explaining brushing techniques in multiple languages or accounting for religious dietary practices that impact oral health. By recognizing these unique needs, professionals ensure equitable health outcomes for children at every stage of development.
Increasing minority representation in dentistry also promotes trust and positive health behaviors in young patients. When children see dental professionals who look like them or understand their experiences, it empowers them to seek care and establish lifelong habits for oral health equity. Modern team-based dental care approaches make use of interdisciplinary teams, combining the expertise of hygienists, assistants, and pediatric therapists with the dentist, enabling tailored solutions for every child.
Institutions developing inclusive dental environments reflect this commitment. Waiting rooms now feature diverse educational materials, gender-inclusive signage, and culturally relevant toys. Dental assistants trained in both technical and emotional intelligence foster an atmosphere of acceptance, soothing children who may be anxious or shy. Through ongoing training, workshops, and exposure to real-life scenarios, dental professionals learn to identify unconscious biases and actively dismantle barriers that have long disadvantaged children from minority or marginalized groups.
New initiatives by dental clinics in 2026 include screenings in nontraditional settings—like Boys & Girls Clubs, refugee centers, and remote community fairs. These efforts not only broaden access to dental care but help families understand the importance of regular visits and preventive measures, ultimately leading to improved oral health education and inclusive dental care for all.
For truly effective pediatric dental inclusion, it’s vital that everyone in the profession—from educators and students to public health specialists and practicing dentists—commits to building a culture of diversity, equity, and inclusion. By adopting these innovations and approaches, dental practices across the country can create profound change, helping every child achieve optimal oral health no matter their starting point.

Professional illustration about Hygiene
Adult Dental Inclusion Cases
A closer look at Adult Dental Inclusion Cases reveals an ever-evolving landscape of both challenges and breakthroughs in advancing patient-centered, equitable care. The push for Diversity and Inclusion within dentistry has rippled outward, making a direct impact on adult patient populations, especially those traditionally marginalized or underserved. For example, adults with disabilities, residents in rural areas, ethnic minorities, LGBTQ+ individuals, and those living in economic hardship often navigate not only barriers to Health Care Access but also implicit biases within the system. Recent initiatives spearheaded by the American Dental Association underscore the integration of Cultural Competence in Dentistry—training dental professionals to understand cultural nuances and social determinants shaping an individual's oral health. This has meant a tangible difference in how adult patients experience care in, say, community dental clinics in urban hospitals versus private suburban offices.
Real-world cases highlight several layers of complexity demanding creative solutions. Consider an immigrant community with limited English proficiency: dentists trained in patient-centered communication and awareness of cultural traditions build greater trust, thus improving oral health literacy and, ultimately, treatment compliance. Similarly, dental assistants and hygienists play an even more prominent role today using culturally sensitive educational materials or arranging flexible appointment times for adults with multiple jobs or caregiving responsibilities. Inclusive dental environments recognize these realities, and many have started implementing multilingual forms, staff from diverse backgrounds, and tailored outreach programs built on community input. Equitable adult dental care now routinely leverages the insights of dental public health experts, cross-referencing scientific evidence with lived experience in their specific locality.
Another significant advancement in equitable care among adults—especially visible since 2026—lies in the proactive hiring and empowerment of a more diverse Dental Workforce. Clinics with intentional strategies to recruit dental hygienists, assistants, and dentists from minority backgrounds have seen noticeable improvements in trust levels and regular attendance among adults in their communities. Minority representation in dentistry addresses more than optics; these inclusivity gains directly correlate to better oral health outcomes. Adults who previously felt alienated due to language, cultural background, or identity now see representatives who both understand their values and affirm their sense of belonging within the dental care system.
Practical strategies are now widely championed by both public and private sectors. For instance, team-based dental care is widely recognized for its benefits in serving complex adult populations by blending the expertise of dentists, hygienists, dental therapists, and public health coordinators. By launching interprofessional case conferences, adult dental cases that may include factors like substance abuse, diabetes, or physical disabilities are addressed holistically. Additionally, more dental education programs and dental hygiene programs are integrating modules dedicated to inclusive dental care, equipping future dental professionals to embrace personalized, respectful care for every adult patient.
The impact of technology cannot be overstated when analyzing the latest adult dental inclusion cases. Tele-dentistry models have enabled both urban and rural clinics to extend their reach, particularly for adults unable to physically access care due to transportation, stigma, or physical challenges. The deployment of these services by a well-trained, diverse workforce ensures that oral health equity is not just a talking point but a deliverable result for adults who have historically lost out in health care disparities. Through these intersecting strategies—ranging from workforce diversity, culturally competent practice, and evolving dental career pathways, professionals provide genuinely inclusive dental care capable of closing the gaps for all adult patients.
The integration and visibility of inclusion efforts in daily practice align closely with modern demands for responsive, modernized dentistry. Whether it's an adult with a chronic health condition seeking preventive dental care without judgment or an LGBTQ+ individual wanting trauma-informed hygiene treatments, today's dental clinics are much better equipped than before. The increased mindfulness toward professional inclusion stands as a defining pillar shaping both individual outcomes and collective uplift toward true health equity within adult dentistry.

Professional illustration about Students
Prevention Strategies 2026
Addressing Prevention Strategies 2026 demands a fresh approach that leverages the combined expertise of dental professionals, revamped education programs, and wide-reaching community outreach. With new findings and best practices released by the American Dental Association and other key authorities last year, dental clinics are now reimagining both introductory and continued preventive care for patients from increasingly diverse backgrounds. Oral health professionals—dentists, dental hygienists, dental assistants, and dental therapists—are broadening prevention efforts with public health initiatives aimed at driving real change in inclusion and health equity. To meet the needs of underrepresented groups, dental care providers now focus on culturally responsive oral health education and team-based dental care.
Strengthening dental inclusion in 2026 begins at the very foundation: educational and workforce pipeline programs. Dental education programs and updated dental hygiene curricula emphasize health disparities, minority representation in dentistry, and cultural competence. These programs include interactive modules on the barriers certain populations face, equipping dental students for patient-centered communication and effective outreach. For example, some dental schools now require immersive rotations in communities with limited health care access so students can better identify social and environmental factors affecting prevention. Likewise, dental public health initiatives champion partnerships with local organizations to foster a sense of belonging. By recruiting and supporting diverse dental students and actively removing obstacles to entry, the dental workforce is projected to become increasingly representative—making patients feel seen and respected as they pursue essential preventive care.
Clinical environments in 2026 are focused squarely on inclusive dental care. Preventive dental care protocols incorporate up-to-date ADA recommendations paired with team-based approaches encompassing dental laboratory technology experts, dental hygienists, dental assistants, and dentists, working together with patients to develop personalized plans. Clinical staff prioritize cultural competence in dentistry, tailored educational materials, and open access channels for feedback, helping ensure that care matches each community’s unique needs. Clinics also roll out strategies like flexible scheduling, multilingual resources, and regular health equity reviews. One prominent practice now integrates community oral health connectors—individuals with strong roots and trust within local populations—who facilitate outreach and bridge gaps in oral health equity. Staff roles are aligned so decision-making reflects true diversity in dentistry, and policies move beyond simple compliance to include regular equity audits and professional inclusion assessment.
Out in the community, the drive to close the gap in oral health leads to robust outreach campaigns featuring preventive education tailored around inclusive dental environments. In 2026, successful outreach features pop-up dental screenings in nontraditional locations—like faith centers, neighborhood markets, indigenous community events, and public parks—expanding preventive dental care into familiar environments without stigma or language barriers. Dental career pathways are spotlighted, letting community members see a reflection of themselves in the dental sector and inspiring the next generation of dental professionals from all walks of life. Educational sessions prioritize topics previously underserved, such as preventative measures for chronic oral conditions linked to broader health disparities, nutritional guidance attuned to cultural preferences, and oral hygiene demonstrations provided by bilingual dental assistants and dental hygienists.
Technology advancements of this year play an outsized role in sharpening prevention effectiveness. With improved digital platforms, clinics and public health agencies engage with patients through telehealth consultations offering accessible advice and at-home preventive tips. Apps in 2026 enable personalized hygiene reminders, easy appointment booking, and even guided routine checks based on individual risk, enhancing the daily practice of preventive care for all. Data tracking empowers clinics to analyze preventive visit uptake across different communities, catching disparities in real-time and adapting outreach accordingly.
For heightened impact, dental education programs emphasize equitable care across specializations. Students participate in collaborative seminars with specialists in public health, social work, and nutrition, jointly designing prevention initiatives. This cross-disciplinary synergy gives rise to innovative strategies—such as using interdisciplinary care coordinating teams in dental clinics, ensuring preventive practices are accessible to underserved populations. Dental hygiene programs place extra value on empathy, belonging, and respectful dialogue to maximize patient connection. With oversight and guidance from bodies like the ADA, dentistry is advancing into a new era, where oral health prevention goes beyond the chair and creates lasting, meaningful change for every community.

Professional illustration about Professionals
Latest Technologies Used
One of the most transformative trends reshaping Dentistry and fostering greater Inclusion in 2026 is the adoption of the latest technologies aimed at creating more equitable Oral Health outcomes. Digital dentistry continues to evolve rapidly, with innovative tools not only improving clinical efficiency but also supporting Diversity in Dentistry and better patient-centered communication, helping Dental Professionals bridge long-standing gaps in Care.
For instance, teledentistry solutions have exploded in use, especially following lessons from recent global health crises and advances in secure digital infrastructure. These platforms not only expand Health Care Access for underserved or rural populations but also create new dental career pathways for professionals, like Dental Hygienists and Dental Assistants, who can now significantly contribute to community education and remote preventive services. Through video calls, remote monitoring, and AI-powered patient assessments, growing numbers of Dental Clinics and Dental Education Programs can engage with diverse communities, see patients previously excluded from traditional dental systems, and deepen belonging within dental public health outreach.
Another groundbreaking tool shaping health equity and inclusion is artificial intelligence-driven diagnostic platforms. Today’s AI imaging software supports Dentists in detecting early signs of oral disease, identifying high-risk patients, and suggesting personalized care plans. What’s uniquely powerful for fostering Inclusive Dental Environments is that these technologies can be trained on datasets reflecting genetic, cultural, and behavioral factors relevant to minority populations, addressing biases that formerly led to health disparities in diagnosis and treatment planning. That means every dental student now learns about integrating AI decision making into equitable care when starting clinical education or Dental Hygiene Programs, fulfilling recommendations from experts like the American Dental Association to hardwire equity into daily workflows.
3D printing and advanced prosthetics are revolutionizing access—even patients previously marginalized because of affordability or custom-fit challenges now benefit from creative Dental Laboratory Technology solutions providing more affordable and individualized crowns, bridges, or dentures. Representing a meaningful step toward Workforce Diversity, many minority-led dental businesses specialize in these services and partner with community health centers, multiplying the reach of Inclusive Dental Care—particularly in cities where diverse patient populations seek culturally sensitive solutions.
In tandem, voice-translated digital patient intake systems and multilingual platforms address a longstanding access barrier, ensuring that diverse patients can describe symptoms, ask questions, and engage with providers in their preferred language. Increasingly common throughout Dental Clinics, these tools foster greater belonging among immigrant communities and ensure no one is left behind simply because their first language isn’t represented among the Dental Workforce. Moreover, culturally-competent AI chat assistants train Dental Assistants and front-office teams in sensitive, patient-centered communication on a daily basis.
On the Dental Education front, immersive virtual reality (VR) and augmented reality (AR) solutions allow dental students—regardless of background—to experience challenging or uncommon procedures thoroughly, thereby standardizing training and reducing competency gaps that can undermine employment and long-term inclusion for underrepresented groups. Likewise, these technologies support collaborative learning: dental students across locations can join shared environments simulating real-world, team-based Dental Care with multiple disciplines represented, reinforcing the value of accessibility and cooperation.
Additionally, the past two years have witnessed significant progress in designing mobile health apps and platforms, focused explicitly on supporting preventive dental care and bridging health disparities. These range from apps that remind patients of at-home Oral Health routines—including communities with lower traditional health engagement—to dashboards used by Dental Public Health teams for tracking regional trends. Many now offer equity metrics, allowing providers to analyze where access gaps or elevated disease prevalence persist and thus direct outreach, resources, and support where they're genuinely needed most.
Finally, forward-thinking clinics now rely on data analytics workflows for evaluating the effectiveness of their inclusion-guided care. By aggregating real-time feedback from patients representing a spectrum of demographic backgrounds and experiences, dental leaders can react quickly if cultural competence, accessibility, or belonging drop—whether it's in provider interactions, Dental Hygiene instructions, or the inclusivity of clinical environments. This approach not only boosts professional inclusion within the team but improves equitable outcomes across the Oral Health spectrum, empowering schools, clinics, and professional associations alike.
The integration of these smart, inclusive technologies marks a critical turning point for Diversity in Dentistry. Ongoing innovation ensures not only the highest standard of care but—most importantly—a firm path toward true oral health equity in America’s ever-changing, beautifully diverse society.

Professional illustration about Dental
Recovery and Aftercare Tips
No matter what type of dental procedure you’re recovering from—especially those performed in settings committed to diversity, inclusion, and health equity—aftercare plays a pivotal role in successful outcomes and patient confidence. Attention to oral health post-treatment can significantly minimize discomfort, optimize healing, and ensure that recovery happens equitably for everyone, regardless of background, physical ability, or access. Even those working directly within the dental workforce, such as dental professionals, dental assistants, dental hygienists, and dentists, are consistently updating their protocols based on guidance from the American Dental Association and leading voices in inclusive dental care for best outcomes post-treatment.
Personalized Aftercare for Diverse Needs
Patient-centered dentistry now goes beyond “one size fits all” instructions. Today’s inclusive dental environments—whether in urban dental hygiene programs, public dental clinics, or private practices—appreciate that each individual’s pathway to optimal oral health is shaped by culture, advocacy, economics, and personal preferences. For instance, multi-lingual aftercare instructions and easy-to-understand pictorial guides help bridge health literacy gaps and empower minority groups often facing health care access challenges. Dental students and dental professionals are now commonly trained to communicate post-treatment steps recognizing familial, linguistic, or accessibility considerations, such as using clear procedure names or listing med doses using plain numbers and visuals.
Tips for Universal but Customizable Aftercare
Detailed, practical tips endorsed by the most current American Dental Association standards and supported by continuous cultural competence training in dental education programs include:
- Pain and Swelling Management: Instructions aren’t just about applying an ice pack or taking medicine. In diverse communities, your provider may offer advice on identifying which over-the-counter medications best align with health traditions, religious beliefs, or sensitivities, plus clarify side effects for different demographic groups often underrepresented in dentistry.
- Braille or Iconic pictographic guides for visual or cognitive/access disabilities ensure every patient gets stepwise reminders for rinsing, brushing, and flossing requirements, correlated with specific recovery stages as charted by dental therapists and dental hygienists.
- Dietary Adjustments: Dental clinics working with community outreach in multicultural neighborhoods offer aftercare diet counseling reflecting cultural staple foods for post-extraction, oral surgery, or trauma patients—like vegetarian-friendly rinses, dairy-substitutes after oral surgery, or highly context-specific soft food lists.
- Positive Reinforcement and Inclusion in Recovery: Messages that instill support and a sense of belonging—such as aftercare care calls in native languages, follow-up emails with personalized video content, and SMS reminders about medication and preventive oral health carea—directly address potential inequities faced by marginalized populations who may otherwise delay seeking care or be hesitant to ask questions.
Facilitating Equitable Health Outcomes: Best Practices in Inclusive Aftercare
Central to recovery consistency is clear team-based dental care. Dental laboratory technology support now commonly tracks personal preferences, mobility challenges, or medical conditions directly in the patient record (with consent), ensuring that recovery recommendations—for “what to eat, when to brush, or when cold packs matter”—align not just with scientific best principles, but also with the realities of varied patients’ lives. Dental professionals today are taught to regularly use patient feedback in post-treatment cycles, which is especially impactful in minority representation in dentistry where one-size-fits-all advice often leads to inequity or treatment discontinuation.
Aftercare communication is steadily progressing. Video demos featuring real patients of different backgrounds showcase universal brushing and medication-taking routines, available in screen-reader optimized formats. Community programs extend care to include ride shares, interpretation services, and outreach calls—all improving follow-through, breaking cycles of health disparities, and confirming oral health equity as achievable in post-operative settings.
Whether you recovered from a clean-up, major orthodontic work, or required comprehensive dental public health outreach casework, these aftercare strategies reinforce inclusion, real-world diversity, and, ultimately, each patient’s return to responsible, resilient, and lifelong oral health and belonging within the wider community. No matter your dentist’s or provider’s background, these actions foster an atmosphere of authentic care, ensuring everyone’s journey through recovery is one of dignity, support, and reliable healing.

Professional illustration about Education
Dental Inclusion Complications
While the recent momentum in inclusion has significantly enhanced diversity across the dental workforce, there remain tangible complications associated with efforts toward dental inclusion—especially as dentists, dental hygienists, dental assistants, and dental public health leaders champion these movements into 2026. Among the most pronounced issues are inconsistent understanding of cultural competence in dentistry and challenges in implementing professional inclusion throughout dental education programs and dental hygiene programs. For instance, despite initiatives by the American Dental Association for oral health equity, disparities persist not only in health care access but also in equitable opportunities among minority groups pursuing careers in dentistry or dental therapy. This is often rooted in implicit bias within both academic admissions processes and the structure of dental clinics, restricting adequate minority representation in dentistry—impacting patients and providers alike. These inequities frequently jeopardize a true sense of belonging and diminish oral health outcomes for patients from under-represented communities.
A further layer of complexity centers on how diversity in dentistry, alone is not enough; inclusive engagement must translate into policies fostering personalized and patient-centered communication. Without strong efforts toward inclusive dental environments, obstacles to equitable care and effective community outreach intensify. Dental organizations that fail to adapt their cultural training for dental professionals can inadvertently perpetuate assumptions and misunderstand cultural, linguistic, or social health differences among patient populations—leading to breakdowns in preventive dental care and reduction in equitable health outcomes. Moreover, disparate experiences among dental students belonging to historically excluded populations often emerge, stemming from the lack of mentorship connections and a fragmentary approach to mentorship by current leadership models within schools and dental laboratory technology settings. Real-world examples, such as difficulties some students face in finding internships or residencies in prestigious dental clinics, speak vividly to these unresolved inclusion challenges even in 2026, hinting at broader infrastructure gaps.
Structural issues across various facets of the dental workforce further fuel complications. Red tape and resistance to modern dental therapy models, sometimes manifested as regulations created without input from dental assistants, dental education advocates, and marginalized providers, constrain effective teamwork and assessment of new solutions that could enhance both care access and professional advancement. There can be friction between efforts to broaden workforce diversity or modernize components of team-based dental care, and resistance from seasoned clinicians hesitant to adapt to change and wholly embrace members new to the field fueled by ongoing myths about qualifying criteria or scope of practice. It's not unusual for dental assistants or those from allied oral health paths, including dental hygienists, to face glass ceilings—even in inclusive-minded organizations—that ultimately cause inconsistency in the delivery of truly inclusive dental care. As of 2026, some dental teams still lack mechanisms for frontline feedback and insufficient resource dedication to oral health education that highlights the nuances of diversity, equity, and inclusion, which collectively shape who succeeds both academically and professionally.
To practically navigate these complications, the American Dental Association, alongside dental schools and community clinics, should focus on multifaceted solutions. These may include dedicated scholarships for students from underrepresented CIH groups, regular staff training addressing embedded prejudices within clinic and education settings, and carved-out leadership pathways designed specifically to amplify the voices of minoritized employees across all dental arenas. Dental career pathways, for example, ought to reflect the reality and values of diverse community experiences; partnerships with local educational providers to ensure inclusion conversations start early will fetch long-term dividends for national oral health. Active participation input from practicing dental professionals—including feedback centered directly on accessibility, safety, or overlooked areas in professional inclusion—should be institutionalized as policy pillars within organizations striving for health equity.
In sum, dealing proactively with dental inclusion complications mandates continuous assessment and introspective program tweaking. It’s essential that every layer of dentistry evolves from dental education and practice leadership to daily hierarchy and patient interaction, effectively creating environments where belonging isn’t a trial but an expectation. While 2026 showcases progress, honest engagement with—and resolution of—existing flaws are vital for the path toward universally accessible, culturally competent, and equitable oral healthcare nationwide.

Professional illustration about Assistants
Finding a Specialist Near You
In 2026, locating a dentist or specialized dental professional devoted to diversity, inclusion, and oral health equity—whether it’s for yourself or your family—has become not only easier, but crucial. Thanks to rapid innovation across the Dental Workforce and heightened awareness about health disparities, you now have a wider range of choices for inclusive dental care ensuring every aspect of dentistry accounts for values like belonging, cultural competence, and professional inclusion. Modern solutions focus on offering patient-centered communication, adaptation for all backgrounds, and an open approach to practice in underserved communities.
Start by exploring established directories offered by the American Dental Association, as they now regularly update listings to highlight providers actively involved in diversity and workforce equity initiatives. Features might also include granular filters based on cultural competence in dentistry, spoken languages, services tailored for people with disabilities, or history in community outreach; thus, you can close the gap in oral healthcare access for traditionally marginalized or minority groups. Dental clinics similarly realize the essential need for greater minority representation in dentistry, to improve consumer choices and promote a stronger sense of belonging. Veterans organizations, urban advocacy projects, and even faith-based community programs right where you live often maintain lists featuring distinguished dentists devoted to advancing grovided-care through diversity.
These new lists might feature practitioners in various roles such as dental hygienists, dental therapists, dental assistants, dentists with backgrounds in dental laboratory technology—not just standard general dentists. For those with distinctive preferences, such as seeking team-based dental care or pediatric or geriatric services infused with focus on health equity, (especially for addressing complex equity dilemmas from youth all the way to older adults), explicit provider profiles featuring inclusion and cultural competency become indispensable. Sleek practice search interfaces now make it easy to glance over providers’ LGBTQ+ policies, experience serving immigrants, advanced DEI (diversity, equity, and inclusion) training, AED access policies, wheelchair navigation, signing services, or multigenerational caregiving—all vital details to ensure that dental inclusiveness keeps pace with societal progress.
For families and individuals striving to identify specialists near them, another practical approach zeroes in on dental education programs—since many prominent colleges create clinically supervised dental clinics as outreach projects within communities known to face health care access challenges. Here, results spotlight ambitious dental students and seasoned educators collaborating around solutions custom tailored for newcomers, racial minorities, or socially or linguistically diverse populations. Community events and pop-up free … Secondary oral health screenings and preventive dental care sessions are often surprisingly helpful for finding relevant dental professionals passionate about health equity.
Given these advancements, also reach for local hospital resources or municipal directories for holistic recommendations linking dental public health experts or practices standing out for specialty care in addition to preventive dental hygiene programs. An increasing number of practices now showcase biographies shining a light on continuous oral health education that promote dental career pathways for learners of diverse profiles. Veterans in dentistry also support equitable health outcomes by designing inclusive environments—think calming decor targeting sensory sensitivities or adult ASD experiences, restrooms dotted with accessibility signage, and clearly described bush-transit proximity for elderly patients—reflecting modernization within 2026 dental public health guidelines.
You’ll unlock genuinely relevant insight by checking reviews online—particularly planet panels and personalized recounts examining whether specific professionals take inclusion seriously and create an environment of real welcome for every patient, no matter demographic factors. Patients should craft useful checklists covering office engagement in diversity training, team language diversity, willingness to build understanding about preferred forms of communication and proactive efforts for connecting community health action goals. Some search depositories specifically tag practitioners based on her participation in coalitions for oral health equity; utilize insurer connections or social health advocates devoted to addressing barriers in preventive dental care.
When searching for dental clinical services grounded in modern inclusion standards without costly premiums, plenty of urban or suburban community clinics operate with pro bono assistance, discounted plans for newly arrived migrants, students, or people moving between insurance gaps, led by professionals recognizing workforce diversity as a strength rather than an add-on. Dig deep into real patient testimonials: Is there sustained effort to reduce health disparities across racial/ethnic barriers, encourage participatory practices, or involve family and caregiver circles in genuine open problem-solving for restorative, esthetic, and longevity-minded dental therapy? Aim for stories not simply describing efficacy, but noting experiential good—forms filled easily, assistance offered to those in need, positive interventions matching inclusive dental environments.
Finally, don’t underestimate the impact of bold professionals willing to reinvent traditional approaches—such as virtual screening conversations and teledentistry. Especially throughout underserved stretches in rural lattices or, paradoxically, in busy metropolitan sections, technology merges convenience and expanded access, connecting dentists supporting disability-access procedures or oral health choices -- enabling current 2026 platforms to unite diverse workforce expertise with patients explicitly uncatered by old mainstream frameworks. Dental inclusion transforms traditional selection in and around dentistry—look beyond sterile institutions, ask within your allied health settings, and inspire newly found ways that honor honest diversity and belonging among providers making real oral health improvements happen.